Patient loads for physicians have steadily increased during the past 15 to 20 years. Currently, they exceed what can be considered reasonable, even for those who feel they can handle 50 or 60-hour workweeks. Figures, published in the peer-reviewed journal Preventing Chronic Disease, indicate that appropriate care for a standard panel of 2,500 patients would take approximately 21.7 hours per day.1 One method has been to involve several members of the practice team to optimize patient outcomes2 while contributing to an improved work-life balance for physicians.
Remote Patient Monitoring (RPM), also known as remote physiologic monitoring (and in some cases remote therapeutic monitoring), can be a major factor in achieving the high-quality care that all healthcare professionals strive to provide. The Centers for Medicare and Medicaid Services (CMS) agrees; they have significantly expanded reimbursement for remote monitoring of chronic and many acute conditions.3
In this article, the Medek Clinical Care Team outlines how RPM is quickly and easily incorporated into the medical practice environment. One positive result is that your staff will become collaborative partners in effective team-based care.
Leveraging RPM to Improve Team Efficiency
Remote patient monitoring systems can include the following devices:
- Blood pressure cuff
- Pulse oximeter
- Weight scale
- Glucose meter
Medek’s RPM devices are very easy for patients and/or their caregivers to use. When patients need help, our team members are skilled at providing additional instruction. HIPAA-secure cellular connections are ready to use as soon as the equipment arrives at your patient’s home. As the prescribing medical provider, you and your medical practice team, will have access to patient data 24 hours per day. In addition, Medek care professionals will monitor patient data and contact your office if any readings fall outside of the norm. Thus, remote physiologic monitoring processes provide an extra level of patient assessment that can dramatically improve your team’s efficiency.
ADDITIONAL RESOURCE: How Can Remote Patient Monitoring Impact Continuity of Care?
Physician as Team Leader
Public health experts see the physician not only as the sole provider delivering care, but as an effective leader who directs and guides other healthcare professionals in achieving positive patient outcomes. Team members can include nurse practitioners, physician assistants, dietitians, and lay coaches.4
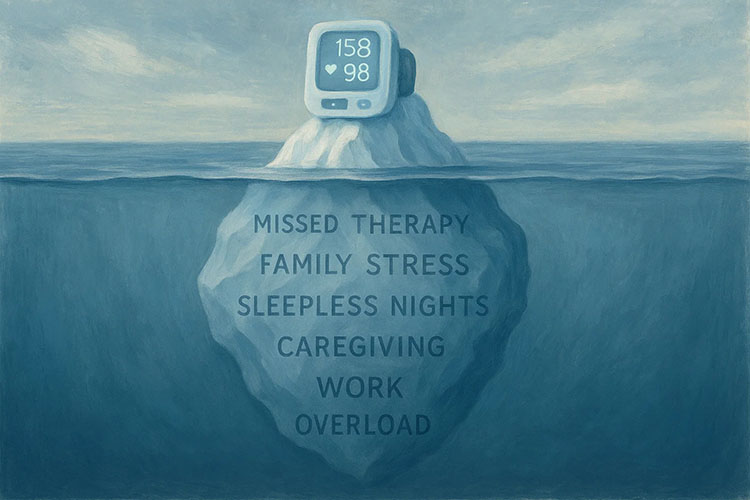
When physicians delegate responsibility for less complex interventions to other professionals, there is more time to treat patients who need physician-level care. Alternatively, it may be the case that a dietitian is better able to provide individualized nutrition education to patients who are struggling with hypertension and/or obesity.5,6 The significance of remote physiologic monitoring is that both a dietitian and the physician will be able to view the patient’s status simultaneously, outside of medical appointments.
ADDITIONAL RESOURCE: Chronic Care Management Gets Better Outcomes with Remote Patient Monitoring
Team Involvement Leads to Empowerment
It is generally accepted that current patient caseloads are simply too large to deliver consistent and high-quality healthcare. Additionally, patients may assume that an appointment with a healthcare professional other than the primary care physician represents a lower-quality interaction, or an unfair cost-saving measure.7
Conversely, studies show that a varied team of nurses, therapists, and health educators often leads to better outcomes and higher patient satisfaction. Although it is likely that most physicians appreciate the value of a team-based approach, in practice, there are few pragmatic strategies for successful implementation.8
The key is the establishment of a common platform for communication, such as RPM. Advanced technology and connectivity facilitate a collaborative atmosphere in which all members of the practice team feel empowered to give each patient their own special brand of excellent care. This is where the advantages of remote patient monitoring strategies are realized. RPM is an implementation tool for coordinated healthcare. When patients see that varied healthcare professionals are knowledgeable about their challenges and successes, they develop increased trust in the entire healthcare team.
In Sum, Many Advantages
We suggest that you view the advanced technology offered by RPM as a communication tool that achieves the following goals:
⇒Provides a common platform for real-time digital communication on the status of your patients for the entire healthcare team.
⇒Reveals how patients are doing outside of the four to five times per year that they come to the clinic for checkups.
⇒Creates an additional revenue stream from Medicare and other insurance providers.
The evidence-based support for RPM should not be overlooked. Multiple studies indicate that the positive effects of RPM are comparable to some hypertensive pharmaceuticals, without any negative side-effects.9
Learning More
Remote Patient Monitoring is an excellent catalyst for team collaboration and time-saving communication. The result will be an increase in positive healthcare outcomes and greater patient satisfaction. We invite you to learn more from Medek consultants about how we can make your life easier while your patients get the care they need.
Request a Demo or Get in Touch
Sources
1Yarnall, K. S., Østbye, T., Krause, K. M., Pollak, K. I., Gradison, M., & Michener, J. L. (2009). Family physicians as team leaders: “time” to share the care. Preventing chronic disease, 6(2), A59. http://www.cdc.gov/pcd/issues/2009/ apr/08_0023.htm
2Hupke, C. (2014, May 16). Optimizing primary care for patients and providers. Institute for Healthcare Advancement. https://www.ihi.org/communities/blogs/team-based-care-optimizing-primary-care-for-patients-and-providers-
3 Centers for Medicare and Medicaid Services. (2020, December 1). Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2021. https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-1
4 Yarnall, K. S., Østbye, T., Krause, K. M., Pollak, K. I., Gradison, M., & Michener, J. L. (2009). Family physicians as team leaders: “time” to share the care. Preventing chronic disease, 6(2), A59. http://www.cdc.gov/pcd/issues/2009/ apr/08_0023.htm
5 Ibid.
6 Hupke, C. (2014, May 16). Optimizing primary care for patients and providers. Institute for Healthcare Advancement. https://www.ihi.org/communities/blogs/team-based-care-optimizing-primary-care-for-patients-and-providers-
7Altschuler, J., Margolis, D., Bodenheimer, T., Grumbach, K. (2012). Estimating a Reasonable Patient Panel Size for Primary Care Physicians With Team-Based Task Delegation. Ann Fam Med, 10:396-400. doi:10.1370/afm.1400. https://www.annfammed.org/content/annalsfm/10/5/396.full.pdf
8 Hupke, C. (2016, January 29). Team-Based Care: Moving from Ideas to Action. https://www.ihi.org/communities/blogs/_layouts/15/ihi/community/blog/itemview.aspx?list=7d1126ec-8f63-4a3b-9926-c44ea3036813&id=1929 AbuDagga, A., Resnick, H. E., & Alwan, M. (2010). Impact of blood pressure telemonitoring on hypertension outcomes: a literature review. Telemedicine journal and e-health : the official journal of the American Telemedicine Association, 16(7), 830–838. https://doi.org/10.1089/tmj.2010.0015