It starts with a data spike…a sudden drop in movement, a rise in reported pain. The alert pings the provider dashboard, hinting at deterioration. But what if that signal isn’t telling the whole truth?
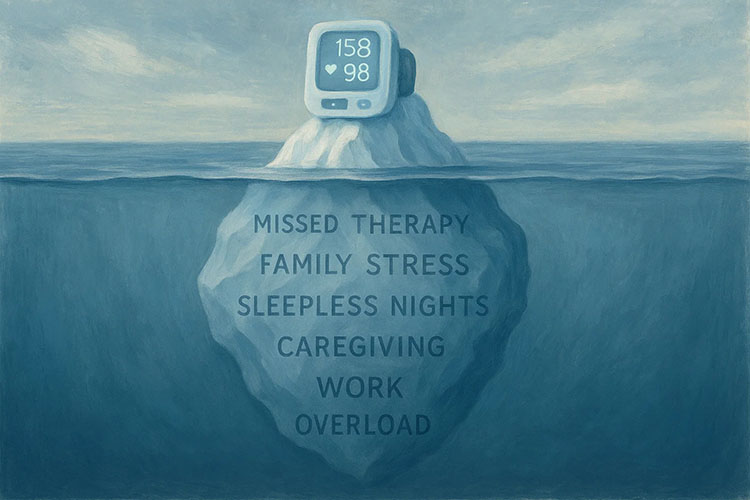
What if that high pain score came after a week of poor sleep, emotional stress, or missed therapy due to caregiving demands? What if the numbers are accurate but the story they tell is incomplete?
Remote Patient Monitoring (RPM) is revolutionizing chronic care, but it risks becoming just another stream of disconnected metrics. Without patient context…what’s really going on behind the data…RPM can lead to unnecessary interventions, missed opportunities, and patients feeling like statistics instead of people.
Let’s look at why RPM needs more than numbers to be effective…and how to make it human again.
The Promise and Peril of RPM
RPM feels like the future. Wearables track blood pressure, glucose, heart rates, delivering real-time insights that catch problems early. CMS reports RPM use grew 200 percent from 2019 to 2023, reducing hospital visits for chronic conditions like diabetes by 20 percent. Doctors get alerts, patients stay home, and practice bill codes like 99457 for the effort. It seems like a clear win.
But there’s a catch. A 2024 Office of Inspector General report revealed 43 percent of Medicare RPM users didn’t receive the full scope of care: device setup, data collection, and treatment management. Data was collected, but care often stalled. Why? Numbers don’t tell the whole story. A spike in Sarah’s pain score could signal a flare-up or just a stressful week. Without context, providers make mistakes, patients feel overlooked, and resources are squandered. RPM’s potential depends on seeing the human behind the data.
The Data Trap: When Numbers Mislead
Data feels like truth. A heart rate of 120 beats per minute looks urgent. But was the patient exercising, stressed, or sick? A 2023 JAMA study found 25 percent of RPM patients felt their data was misinterpreted because providers didn’t ask about their lives. RPM systems churn out metrics but rarely capture context like stress, sleep, or social challenges. This gap leads to misdiagnoses, unnecessary interventions, and frustrated patients.
Billing suffers too. Practice administrators know RPM codes require 20 minutes of clinical time monthly. But if staff only react to data without engaging patients, they miss billable care coordination, like discussing Sarah’s therapy lapse. A 2024 HFMA report noted 30 percent of RPM claims face denials due to incomplete care delivery. Data driven care sounds advanced, but it falters without the human element.
Reframing RPM: Care, Not Just Data
Making RPM work means prioritizing humanity over tech. Start by inviting patients to share context with their data. Asking “What was happening when your readings spiked?” can change everything. A 2023 study showed patient engagement in RPM boosted adherence by 30 percent. Picture nurses guiding Sarah to log stress alongside pain scores, giving her doctor a clearer view.
Next, blend lifestyle factors into RPM platforms. Some systems now let patients note events like missed therapy or family stress. This contextual data helps providers make smarter decisions, reducing errors by 15 percent, per a 2024 study. Regular check-ins are just as vital. A five-minute call can clarify a data blip, like whether Sarah’s low activity was a health issue or a busy week. Practices that added calls saw 25 percent higher patient satisfaction.
Chronic conditions often intertwine with mental health. Pairing RPM with behavioral health screening cut perceived pain by 25 percent in a 2024 study. If Sarah’s stress is amplifying her pain, a counselor’s input could matter as much as her meds. Finally, consider access. Rural patients, 20 percent of whom lack broadband, miss out on RPM. Offering phone based check-ins ensures everyone benefits, with practices seeing 10 percent more patients enrolled.
RPM Done Right
Take a real-life scenario: a patient’s RPM device flags rising pain and declining activity. Instead of immediately adjusting medications, a nurse reaches out. The patient shares that they’ve been dealing with a personal crisis and missed therapy sessions. With that context, the care team adjusts the plan…adding a counselor referral and support reminders…without jumping to conclusions. That one call, driven by data but rooted in understanding, keeps the patient on track. Their pain stabilizes, and they feel seen.
The Bigger Picture: Trust Over Tech
RPM’s future isn’t about smarter devices… it’s about trust. Patients want to feel seen, not reduced to numbers. Providers need tools that simplify care, not complicate it. Administrators want billing that flows. A 2024 survey found 60 percent of RPM patients felt closer to their care team when context was part of the process. That’s the vision: technology that amplifies care, not overshadows it.
This matters beyond clinics. As value-based care grows, with CMS aiming for 100 percent of Medicare payments to be value-based by 2030, RPM will be judged on outcomes, not just data points. Practices that humanize RPM now will reduce readmissions, lift satisfaction, and secure revenue.
The Catch: It’s Not Easy
Humanizing RPM requires effort. Training staff to engage patients takes time. Upgrading platforms to include lifestyle data can cost $10,000 to $50,000 for small practices. Creating equitable solutions, like low-tech RPM, demands new workflows. But the rewards are clear: practices prioritizing context in RPM saw 20 percent fewer denials and 15 percent higher revenue in 2024.
Your Next Move
Transforming RPM starts with small steps. Add a prompt to your RPM system, asking patients what was happening during their readings, and review responses for a few patients to see how it shapes care. For the next RPM alert, call the patient to clarify, noting if it prevents an unnecessary visit. Train a nurse or coordinator to weave context into RPM reviews, tracking time and feedback after a month. Review last quarter’s RPM denials to spot missed care coordination and adjust workflows.
A practice that added patient check-ins cut denials by 10 percent in three months. These steps are simple but powerful, paving the way for care that’s as compassionate as it is smart. Share your thoughts below or try one idea and see the difference. Let’s make RPM human again.