Before the pandemic, Remote Patient Monitoring (RPM) seemed futuristic and costly. Now, COVID-19 opened the industry’s eyes to telehealth services and remote care possibilities. One of the biggest benefits of this innovative technology is its impact on our public health.
Healthcare Inequities
In the United States there exists underserved healthcare communities. These may be low-income areas. The people in these areas have an increase of chronic illnesses. These may include heart disease, diabetes, and obesity.
Adding to this problem is a shortage of medical services in these areas. People in low-income communities may not have private health insurance. They may rely on Medicaid and Medicare. Without private insurance, people often put off or delay the medical care they need. This is especially true for their chronic illnesses.
These healthcare inequities have an economic impact on our nation as well. The Kaiser Family Foundation created a report that states inequities in healthcare cost the country. It projects that around 93 billion dollars are spent in excess medical expenses per year.
During the pandemic, the Centers for Medicare and Medicaid Services (CMS) made changes. They changed the payment rules for telehealth and remote patient monitoring services. This will benefit all public health efforts, including those in low-income communities.
Remote Patient Monitoring During a Public Health Emergency (PHE)
During the pandemic, the importance of Remote Patient Monitoring became evident. At the pandemic’s peak, those with chronic illnesses could not go to a doctor’s office or hospital. Their chronic illness meant they were at greater risk of getting Covid. They had a greater need to remain on lockdown at home. This continues, even as restrictions lessen.
Because of the issue, the CMS issued an interim rule. It gives healthcare providers more flexibility in using remote care. This includes telemedicine and Remote Patient Monitoring.
The question of consent was important to the CMS. They agreed that consent could be given remotely. Virtual care needs this type of consent. The CMS stated that practitioners could provide RPM services for acute and chronic conditions independent of the PHE.
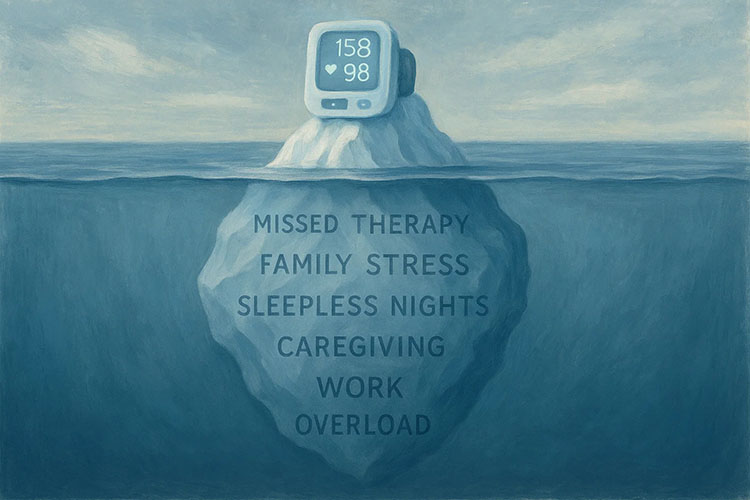
Managing Chronic Illnesses
The initial surge in services was telehealth visits. Telehealth is an office visit done virtually. This can put doctors in rural areas where there were none before. In locations where people have to travel hours to get to a hospital, Telehealth clinics could be established. This expands access to healthcare. They could also provide visits to people’s homes. Yet, clinicians need a more continuous approach to chronic care management. That is where Remote Patient Monitoring becomes relevant.
Remote Patient Monitoring, or RPM, is when patients use a medical device in their home. The information from that device is sent to their doctor via a secure connection. This can offer daily healthcare information to a doctor located miles away. Connected medical devices might include:
- Glucometers
- Blood pressure cuffs
- Weight scales
- Pulse Oximeter
RPM is critical in seeing trends in a person’s health. It can measure how effective medicine or treatments have been. It provides valuable healthcare information for better treatments.
RPM opens up new options for providers, too. Physicians are not necessary to manage remote patient monitoring. A Nurse Practitioner, a Physician’s Assistant, or a third-party service can do the monitoring. These healthcare professionals work under the supervision of a physician (MD or DO). With telehealth and RPM, technology can help care for patients who had no access to a doctor before.
Bringing Broadband to Underserved Communities
The benefits of RPM and telehealth services go beyond healthcare, too. Underserved communities not only lack healthcare services but technology services, as well. Internet and broadband services may be lacking or very limited.
To fix this problem, several groups are working together. State government, local communities, and private organizations have joined together. Their effort is to bring affordable broadband to these communities. They are trying to bring affordable access to these communities. Better access to technology means better healthcare options. This includes access to remote patient monitoring.
Any plan to help improve health services to remote areas must include a Broadband initiative. This will have a rebound effect in other areas. Increased broadband access will lead to better health outcomes. These may include lower rates of smoking, less obesity, and reduced diabetes. People eating more fruits and vegetables is an indirect benefit, according to a 2012 study published in Behaviour & Information Technology.
Introducing new healthcare options to underserved communities impacts overall public health. Remote Patient Monitoring needs to be a vital part of making this happen.
Medek RPM is a national leader in the field of Remote Patient Monitoring. Start a conversation with a Medek Representative today!