Fifty percent of the U.S. population requires Chronic Care Management (CCM), according to a 2020 report published in ACR Open Rheumatology. Today’s healthcare seeks to help these patients while lowering costs without affecting the quality of care. One way to reduce expenses and improve care quality is with Remote Patient Monitoring (RPM) and its technological advances.
The Importance of Chronic Care Management
More and more providers are implementing Chronic Care Management into their practices as the population ages. CCM is a non-face-to-face visit typically provided to Medicare patients with multiple chronic conditions, including diabetes and cardiovascular disease.
CCM offers valuable benefits:
- Care Coordination Organization becomes challenging when the patient has to manage multiple illnesses. They may seek multiple providers regarding different issues. For instance, patients may see a dietitian for their diabetes management and a cardiovascular specialist for their heart disease. Structured CCM allows all the care team members to stay actively engaged with the patient. Each provider gets a complete picture of the patient’s health status.
- Increased revenue streams – Since 2015, the Centers for Medicare & Medicaid Services have offered a reimbursement program for CCM. That means providers get additional revenue for providing patients services that benefit them. CCM fits tightly into the value-based care model while offering healthcare providers an additional revenue stream.
- Quality of life – Chronic illness can significantly impact patients’ quality of life. With Chronic Care Management, the care team provides much-needed attention to each patient, reducing depression and improving pain management. That may mean patients can be more active and participate in more social activities with family and friends.
Moving RPM Into the Forefront of Chronic Care Management
In 2020, CMS also created policies for Remote Patient Monitoring (RPM). The agency will reimburse private practices that engage remote treatments using devices to collect essential physiologic data and then provides RPM billing codes in their billing.
One thing the pandemic did was prove the effectiveness of Remote Patient Monitoring. Practices had to learn to reach out to patients without having them come to the office, especially those with chronic illness and at high risk of severe COVID-19 complications.
At the same time, it introduced the power of Remote Patient Monitoring to practices that had previously avoided it. Through Remote Patient Monitoring, clinicians get a holistic view of their patient’s health over time. This increased visibility helps to ensure the patient’s adherence to treatment and allows for necessary interventions. RPM also will enable practices to build better relationships with their patients and to develop a more personalized care plan. This is true even for patients without chronic illness.
It doesn’t take costly equipment or lots of space. All practices need is a virtual platform able to sync with mobile devices.
How RPM Improves Chronic Care Management
With RPM, clinicians can collect and share biometric data and patient-reported insights with care team members. That allows for a better evaluation of trends. It also allows for enhanced patient education and engagement. Care team members can use the data to identify behavior changes and improve self-care. RPM can be part of treatment plans for many of the most common chronic illnesses.
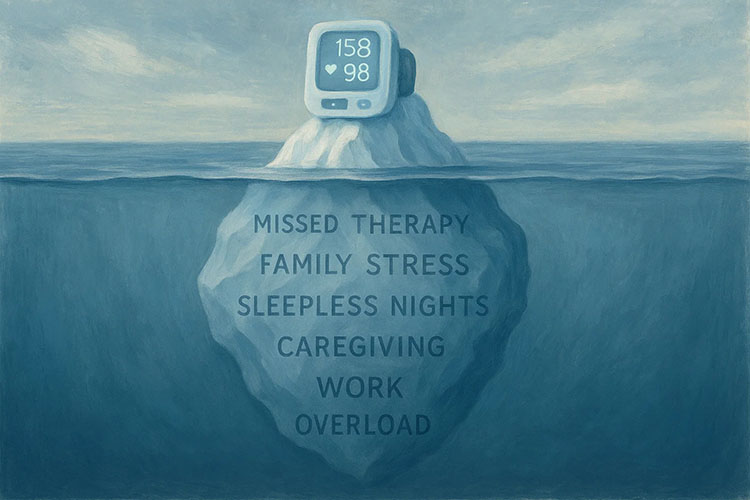
Hypertension
The American Heart Association reports that the age-adjusted prevalence of hypertension in adults is close to 35 percent or about 85 million people. By 2035, that number will be closer to 42 percent just in the U.S.
Studies have proven RPM can dramatically lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) compared to standard treatment and self-monitoring alone.
Heart Failure
Heart failure is responsible for high rates of hospitalizations and readmissions in this country. Although there are limited studies about the effect of RPM on heart failure, the data that is available indicates it is beneficial.
A-Fib
Non-randomized trials show that RPM has the potential to enhance outcomes by enabling accurate and early diagnosis and lowering all-cause mortality and hospitalization rates. Therefore, recent clinical guidelines strongly advise using RPM to diagnose AF in stroke and non-stroke patients.
Diabetes
Diabetes care relies heavily on adherence to strict care guidelines. With RPM, patients can see the results of their self-management and may be more likely to avoid complications. Telehealth and RPM also provide more access to care for those in underserved communities often inflicted with the condition due to poor diet.
As practices seek better patient outcomes while reducing costs and adding additional revenue streams, RPM and CCM become valuable tools for patients and practices. Technology has removed barriers that previously prevented greater adoption. RPM and CCM are not trends of the future, they are needed services for today.
Medek RPM is a leader in the industry, helping patients and providers. Start a conversation with a Medek Representative today!